The catastrophic failure of many Western democracies such as the U.S., UK and many European countries to control COVID-19 has been shocking.
Prior to this pandemic, there has been a long-held view in these same countries that only fragile states and low-income countries will fail during a pandemic, and would need benevolent assistance from high-income countries. This is best reflected in the 2019 Global Health Security Index (GHSI), launched a few months prior to the pandemic and ranking the U.S. number one in preparedness.
Low-income countries which have controlled COVID-19 well – such as Vietnam and Samoa – were ranked 50 and 162 respectively. Samoa simply closed its international borders — something which the World Health Organisation (WHO)continued to insist should not be done. Border closure is also the secret to the success of New Zealand and Australia in keeping their countries relatively COVID-free.
The state of the pandemic in the U.S., UK and Europe shows that money, technical know-how and scientific knowledge do not guarantee good pandemic control. Culture, leadership, appropriate experts informing policy decisions and the willingness of the public to follow expert advice matters too.
Countries which share these characteristics have done better — ranging from communist states such as China and Vietnam to small pacific islands like Samoa, to democracies such as Australia and New Zealand. In these countries, the pandemic was brought under control with routine evidence-based public health measures such as border closure, case finding, contact tracing, quarantine, social distancing and lockdown.
Civic mindedness and trust in government have also proven to be of major importance in pandemic control. Australians and New Zealanders tend to trust the government and largely followed public health orders. In contrast, there has been resistance to public health orders in the U.S. and UK.
We have seen the dire outcomes of poor leadership in the U.S., where leaders have peddled unscientific theories, deadly miracle cures and actively discouraged public health interventions such as masks and social distancing, fanning mistrust. This has resulted in basic public health measures such as masks and vaccines being politicised and seen as symbols of oppression in the U.S. The lasting damage and mistrust will also make high vaccination coverage rates and herd immunity much harder to achieve in the U.S.
Pandemic control requires appropriate expert advisors with epidemic control experience to lead control efforts. Yet public health is invisible compared to clinical medicine and political leaders may fail to appreciate the importance of getting proper expert advice.
I could pretend that my specialist medical qualifications make me a good choice to treat an acutely ill patient in hospital and the patient may not know the difference, given my qualifications on paper seem appropriate. I would not dream of posing as an expert in areas which I am not current or expert in — yet we have seen exactly that happen during the pandemic.
Clinicians and basic scientists have been favoured over public health experts on pandemic planning and expert groups around the world since the 2009 H1N1 influenza pandemic, leaving many such committees without the requisite knowledge of public health epidemic control. Clinicians, basic scientists and hospital infection control experts have been steering major decisions, without the input of experts in population-based epidemic control measures or other relevant experts from other disciplines.
An example of failure to utilise relevant expertise is the denial of the importance of airborne transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by experts on the WHO infection control committee. The evidence is clear that SARS-COV-2 is airborne, yet guidelines in many countries do not yet reflect this, thus hampering the ability to control the spread and endangering health workers.
No aerosol scientists or engineers who understand the transmission of respiratory viruses and movement of aerosols are on the WHO committee, and their expertise not sought, prompting calls from scientists for WHO to acknowledge airborne transmission — all while the pandemic continued to spiral out of control despite handwashing and social distancing.
Control of SARS-COV-2 requires multidisciplinary expertise, yet was led by infection control experts whose bread and butter is control of wound infections and antimicrobial resistance — for which handwashing is key. The lack of experts on respiratory transmissible infection or aerosol science at the table meant that much of 2020 was spent on promotion of hygiene theatre, actively discouraging mask use and a resulting low awareness among the general public of the importance of ventilation and masks in reducing their personal risk.
Many politicians and the public do not understand “public health” and equate it with the provision of acute health care in public hospitals, or confuse it with primary care. In brief, public health is the organised response by society to protect and promote health and to prevent illness, injury and disability.
Public health comprises three main components:
- Health protection — the use of legislation such as the banning of smoking in public places, seatbelt legislation and food labelling or emergency powers which allow pandemic control measures such as lockdowns.
- Health promotion — the process of 'enabling people to increase control over and to improve their health'. An example is the promotion of masks and social distancing.
- Disease prevention and early detection — this includes surveillance, screening and prevention programs. An example is wastewater surveillance for SARS-COV-2, which can provide early warning of community transmission of COVID-19. Vaccination programs are an example of disease prevention and are one of the most successful public health interventions in history, with achievements such as eradication of smallpox.
Public health requires specialised skills, training and a skilled workforce. During the pandemic, we have seen resources committed to surge capacity for clinical medicine, but there has been a lack of understanding of the need for public health surge capacity.
In Australia, we had an expansion of intensive care unit (ICU) and hospital capacity in March, in preparation for clinical surge, but the second wave in the state of Victoria was fuelled by the lack of surge capacity in contact tracing and outbreak investigation, which had not been identified as a separate requirement. This lack of recognition left hospitals and primary care physicians to organise their own contact tracing.
The specialised public health expertise in pandemic control lies with those who are trained in field epidemiology, an under-recognised discipline within public health. Field epidemiologists are trained in the science of detecting, preventing and controlling epidemics and are well versed in core concepts of successful epidemic control such as contact tracing and case finding.
We have a global network – Training Programs in Epidemiology and Public Health Interventions Network (TEPHINET) – of Field Epidemiology Training Programs (FETP), which are a specialised workforce program spawned from the United States' Epidemic Intelligence Service (EIS) training program of the Centers for Disease Control and Prevention — a program developed in 1951 in response to the threat of biowarfare.
Outbreak investigation, disease surveillance, prevention, field response, contact tracing, risk assessments, use of vaccines to control outbreaks and other aspects of outbreak control are core competencies in field epidemiology, which is an essential speciality for pandemic control.
Currently, there is no data on the efficacy of COVID-19 vaccines used as post-exposure prophylaxis, when many vaccines have efficacy when given to close contacts. This strategy was first developed for smallpox eradication when mass vaccination posed a challenge in India. It turned out that smallpox vaccines had about a halving of efficacy – from 97 per cent to 50 per cent when given to exposed contacts – but this was enough to complete the eradication of smallpox.
Ring vaccination requires contact tracing and vaccination of contacts, but contact tracing has all but been abandoned in the U.S .and UK. There is no research on the use of COVID-19 vaccines as post-exposure prophylaxis in contacts, but we showed this would be the best use of a limited vaccine supply during an outbreak.
While contact tracing became a mystical revelation to nouveau experts in 2020, it is routinely used by outbreak teams for many serious infections such as tuberculosis, meningococcal disease, measles or hepatitis A. Contact tracing is conducted because close contacts are at the highest risk of becoming infected next and if they are not identified and quarantined, will go on to infect others and cause exponential epidemic growth.
Contact tracing is feasible for SARS-CoV-2 due to the long incubation period — the long incubation may also make vaccines effective in contacts. Yet in February 2020 in the UK, the Scientific Advisory Group for Emergencies (SAGE) committee in the UK stated they would cease contact tracing if the epidemic became too large.
In the U.S., a pragmatic decision was made (presumably in the face of an insurmountable task in contact tracing and monitoring) to reduce the period of quarantine to one week. The rationale for abandoning or reducing contact tracing is the intensive human resources required to contact trace ten to 20 contacts per case when an epidemic becomes too large.
If 10,000 cases a day are occurring, that equates to 100,000 to 200,000 contacts per day and up to a million contacts being monitored at any one time during quarantine. Contacts need to be traced within 24 to 48 hours to stop them from infecting others. However, a range of digital contact tracing methods – such as Apps, QR codes and tracking digital footprints through other means – can be used to overcome the lack of human resources.
In Wuhan, when the epidemic grew too large and manual contact tracing became unfeasible, the use of digital tracing was highly successful. All efforts should be made to complete contact tracing, as it is highly influential in epidemic control.
The lack of public health input has also resulted in unscientific theories and poor management being pushed in many countries by expert groups — such as the “herd immunity by natural infection” theory which has become a household narrative during the pandemic despite being unscientific.
Herd immunity is a concept which arose from vaccine programs and anyone with knowledge of the pre-vaccine epidemiology of infections now prevented by vaccines understands that no infection ever controlled itself without the use of vaccines. Smallpox caused recurrent, large scale cycling epidemics in the pre-vaccine era, as did measles.
Finally, clinician advisors who do not understand non-pharmaceutical epidemic control measures turn to medical technology as the only familiar solution. Recently, for example, the UK was recommending blanket testing of everyone in an entire city — another shot-gun approach reflecting lack of knowledge of non-pharmaceutical epidemic control.
The pandemic spiralled out of control in the UK because someone thought the school holidays were enough of a circuit breaker to allow a jolly holiday season (while telling us through most of 2020 that kids do not transmit and schools should stay open) and now the Variant of Concern 202012/01 (B117) is spreading around the world.
In response, the UK decides to test incoming overseas passengers. That's akin to setting up a smoke alarm in the next suburb in response to your kitchen being on fire and allowing the whole house to burn down in the process. Testing outgoing passengers leaving the UK would do much more for pandemic control.
To confound things even more globally, there has been a pandemic of "experts" commenting in the media, unashamed to discuss anything – even subjects they have zero track record in – and therefore providing the public with garbled and misleading messages. I have seen non-clinicians with no track record in treatment, who have never stepped inside a hospital or treated a patient, happily discussing drugs and vaccines.
Every doctor, professor and epidemiologist, it seems, has come out seeking to posture and pose as an expert in pandemic control. This has led to confused and brand new terminology being used during this pandemic, like "vaccines stopping transmission". Vaccines work by preventing infection. Sometimes they do not prevent infection, but still reduce disease severity should you get infected.
This is the distinction they mean when they talk about "preventing transmission". If a vaccine prevents infection, it will prevent transmission — and this is where fake experts have become confused and created a new, mainstream narrative. Sadly, these experts are so powerful that I have heard genuine vaccine experts start adopting this terminology.
During COVID-19, government advisors without training in epidemic control have learned the basics along the way, as the pandemic unfolded, at great cost globally. There are many different disciplines relevant to pandemic control, including the sub-specialities of clinical medicine, epidemiology, basic science, drug development, public health, occupational health and aerosol science — all of which are needed to bring this pandemic under control.
Like aviation, each area is equally critical, but if public health, field epidemiology, aerosol science, occupational hygiene and engineering are not represented on decision-making bodies during the pandemic, accidents will happen.
Just like accidents may happen if I turn up at the operating theatre to conduct surgery on some unsuspecting patient because I have a Bachelor of Medicine and Bachelor of Surgery, did well in anatomy during medical school and assisted in some operations as a resident. I might have enormous faith in how fabulous I am and have no regard for the expertise of real surgeons ("It's just a gallbladder. How hard can it be?") and you may not know the difference — but is it acceptable?
This has happened exactly with the pandemic globally, with extremes such as a radiologist being put in charge of the U.S. pandemic response, to more subtle examples where people with some tangential expertise in epidemiology or infectious diseases (but not in epidemic control) are driving disease control policy, making up new terminology, confusing and confounding the public or pushing dangerous manifestos.
The same people who peddled herd immunity by natural infection are now silent on herd immunity by vaccination being a feasible goal. Instead, they are telling us "we have to live with COVID-19" and giving negative, defeatist messaging to us.
Countries that use a high efficacy vaccine and achieve high vaccine coverage may feasibly achieve herd immunity and eliminate sustained community transmission, yet only a few countries like Israel are conducting ambitious, determined, organised drives for mass vaccination.
Why did this hijacking of public health happen? As someone who has worked in pandemics and epidemics for 28 years, I have noted a shift since the 2009 influenza pandemic. Although it was a mild pandemic, the response to that was more organised, informed and traditional in the U.S. and UK than the COVID-19 pandemic.
I believe, being the first "modern" pandemic, it shone a light on the opportunities that pandemics and serious epidemics provided for career advancement — opportunities which had dried up in other areas of infectious diseases.
The hijacking of public health has been a gradual occurrence since then, so that now, during the worst pandemic of our lifetimes, we have a loss of core public health expertise in decision-making bodies. So, governments have not been well advised and have repeated what they have been told — that we can live with COVID.
In a pandemic, the health system is the weak link in society. Every country that has resisted lockdown and insisted life go on as normal has been forced into lockdown when exponential epidemic growth has caused the health system to collapse. When bodies were piling up, ventilators had run out and health workers were dying.
Pandemic control requires specific skills and knowledge and when people without these skills are driving the response or posing as experts, it’s akin to an air traffic controller flying the plane. They may be smart and have some relevant knowledge but will have to learn as they go and may make mistakes, sometimes catastrophic.
A pandemic is no time to give non-experts – who think that they should be in charge – a crash course in epidemic control. Because of exponential epidemic growth, time is of the essence. Without this, many health systems have become overwhelmed as the pandemic surges globally.
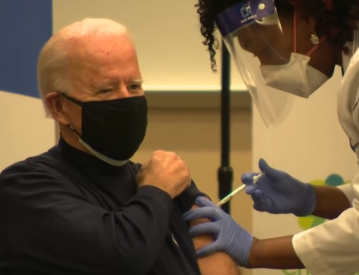
Vaccine roll-out programs – the only hope in countries that have abandoned basic epidemic control such as contact tracing – are coming unstuck because the scale of the undertaking was not appreciated. Sadly, this is a lesson that had to be learned in real-time during the pandemic because of the lack of a full spectrum of experts providing advice to governments in many countries.
Professor Raina MacIntyre is Professor of Global Biosecurity and National Health and Medical Research Council (NHMRC) Principal Research Fellow. She heads the Biosecurity Program at the Kirby Institute. This article was first published on NHMRC Centre for Research Excellence Integrated Systems for Epidemic Response (ISER) under the title 'The Hijacking of Public Health and the Price Paid During the COVID-19 Pandemic' and is republished with permission.
Support independent journalism Subscribe to IA.