Damage done by the COVID-19 pandemic was worsened in Australia due to a lack of preparation and effective management, writes Dr Kim Sawyer.
WHEN I FIRST WROTE of the pandemic, I looked back at Australia’s pandemic management plan of August 2019. The plan tells more from what it does not say rather than from what it says. There is no mention of lockdowns. There is no mention of purpose-built quarantine facilities. There is only one reference to aerosols. We were on the back foot at the start. We stayed there. We did not have a real plan.
We were distracted by the World Health Organisation (W.H.O.) naming the disease COVID-19. The virus is SARS-CoV-2, but the disease COVID-19. The disease was distinguished from SARS to prevent fear in countries that experienced SARS. That may have been a mistake. Perhaps it should have been called SARS-2. We may have understood better.
Three important attributes of COVID-19 were underestimated. They never should have been. The virus hides better than most viruses. Most of those infected will never show symptoms. The virus spreads through the air in aerosols, often at distances much greater than 1.5 metres. Not everyone who contracts the virus spreads the virus, but some become the super spreaders. All of this was known from the early studies in Wuhan, yet for some reason, they were ignored. That was a mistake. It is the key to fighting the virus.
The asymptomatic are the key. They are the spreaders. An early study showed an asymptomatic carrier travelled from Wuhan to Anyang. She infected five relatives and two were admitted to intensive care. Yet the carrier showed no symptoms. She tested positive only once in four tests. The virus hides very well.
In March 2020, I wrote that we needed to sample across the population, find the spreaders before they spread. We need to sample the virus, not let the virus sample us. We could have used antibody and antigen tests to increase the power and frequency of testing, as a Cambridge University study showed.
Instead, we opted to use only one test, the PCR (nose swab) test. That was a mistake. It is the same mistake we are making in 2021. There are rapid tests being used in the U.S. and UK where people can test themselves at home as much as several times a week. The frequency of testing matters. We need to begin rapid testing, particularly in high-density areas like universities and apartment complexes.
Aerosols are another key. Quarantine breaches are attributable to aerosols and poor ventilation. I wrote in July last year that the story of aerosols was told by SARS in two hospitals in Vietnam in the 2003 outbreak. In the modern air-conditioned hospital with closed windows, extensive transmission of SARS occurred. In a second hospital with ceiling fans and large windows kept open for cross-ventilation, there was no transmission. I wrote then that we should not quarantine travellers in closed, air-conditioned buildings, but in buildings where the windows open and away from population centres. It was the first lesson of SARS.
There was another lesson of SARS. We need to separate COVID-19 patients from others — not just a different floor of the same hospital, but in a dedicated facility. In Melbourne last year, I knew of two individuals who were admitted to hospital for minor procedures. They contracted COVID-19. We must consider using only one dedicated facility for treating COVID-19 patients in each state. We must find ways of ensuring the ventilation is as good as in the second hospital in Vietnam.
We have assumed that every person who gets the virus will spread the virus. That is not right. The virus spreads through explosive clustering. Studies show that ten to 20 per cent of the infected are responsible for 80 to 90 per cent of the transmission. Many do not transmit at all. SARS was the same. It means we need to identify the super spreaders before they spread.
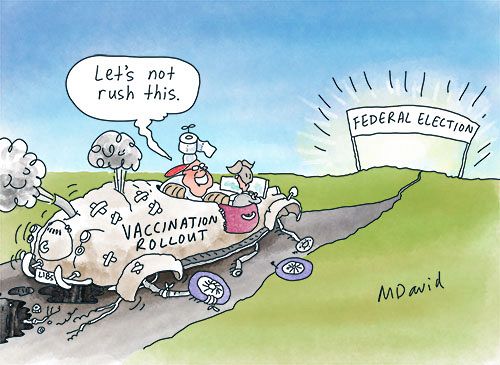
In 2020, there was an imperative to identify spreaders. In 202, there is an imperative for spreaders to vaccinate. Vaccination reduces the probability of contracting the virus. Vaccination also reduces the probability of transmitting the virus. The vaccination program should be extended to include the younger, more mobile and socially interactive population. We must vaccinate to protect the vulnerable, but we must also vaccinate to prevent the spread. It means allowing younger people to be vaccinated now. We need to be pre-emptive.
The risk in Australia was always going to be low due to our population density and air quality. Being an island in the Antipodes was our greatest advantage. The countries having the lowest infection and mortality rate are islands. But being complacent has been our great disadvantage. The complacency has been self-evident. The virus did not go away, it just hid better. The viral load was too low to be detected, but the virus was still present in wastewater samples. It is the same across the region. In Singapore, Taiwan and Thailand, it has re-emerged.
We now need to look forward with a pre-emptive strategy to prevent a third wave of infection. We know more than we did last year. We now understand the importance of the asymptomatic carriers who are potentially super spreaders. We now understand the importance of aerosols. There are two policies that we can now adopt.
The first is the rapid testing being advocated by the U.S. Centre for Disease Control (CDC). Rapid testing should be adopted for those in quarantine and in the month after quarantine. Rapid testing should also be used in high-density populations like universities. It may identify explosive clusters before they form. It may prevent lockdowns.
The second policy is to extend the vaccination program to the under-40s. We cannot afford to wait for the Moderna vaccine in December. We need to give the population that is most mobile the opportunity to be vaccinated. It is the logic of being ahead of the curve of infection.
Australia did not have a real pandemic plan. The virus had us on the ropes right from the start. We can do better.
Dr Kim Sawyer is a senior fellow in the School of Historical and Philosophical Studies at the University of Melbourne.
Related Articles
- Tokyo 2021 Olympics could become a test of governmental hypocrisy
- Above all, 'COVID truther' groups are tragic
- COVID-19 vaccination should not encroach on civil liberties
- World travellers: Back to the future after COVID-19
- Australia still among lowest in COVID-19 deaths as global trend improves
 This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Australia License
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Australia License
Support independent journalism Subscribe to IA.